
latest
Research and Commercial Use of Healthcare Data in Uncertain Times

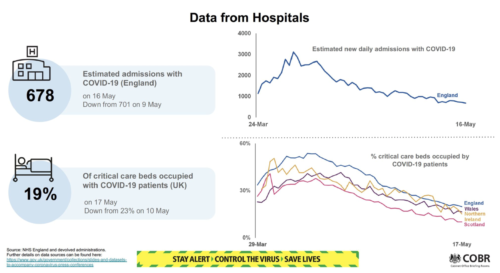
The value of healthcare data has, potentially, never been more widely recognised than it is now in the context of COVID-19. Around the world, it is being put to work in the service of prevention (wash your hands!), to understand and improve the treatment of patients affected by the virus, to help design safeguarding measures to protect health workers and those in their care, facilitate healthcare system management as well as to enable important research and innovation. In the UK, its presence is felt by us all – appearing front and centre at the daily No 10 press briefings as well as in graphs and charts that have come to dominate the media in recent months.
It is, perhaps, understandable that aspects of our data-driven efforts to tackle the emergency whilst being ‘led by the science’ should have courted controversy: that we live in inherently uncertain times seems, at times, the only real certainty and uncertainty has a distinct tendency to give rise to anxiety.
From impatience with gaps in our understanding about the people affected by COVID-19 and impacting whether, when and how to lift various aspects of the recent lockdown, to concerns about the use of data by people leading and involved in everything from pandemic modelling efforts to delivering the UK’s ‘track, test and trace’ capability, healthcare data is headline news.
How are we to build and maintain public trust in its use without applying (too forceful) a brake on research, innovation and the goal of supporting improved care against this unprecedently ambiguous backdrop?
Business as Usual or Unusual Business?
The decisions being taken to expedite data usage during the public health emergency are increasingly subject to scrutiny by civil society organisations. In particular, where that use will involve non-governmental actors, they seek to understand the rationale for using healthcare data, the design parameters of diverse systems and applications, as well as the terms and conditions of agreements entered into with third parties. These themes are articulated following the passage of emergency legislative provisions, the issuance of Control of Patient Information (COPI) notices by the Secretary of State for Health and Social Care (whose effects include requiring information sharing by pertinent public bodies and suspension of the Duty of Confidentiality in the public interest to enable direct care as well as research) and associated regulatory changes. These are highly unusual circumstances, then, whose longevity and long-term implications are currently unknowable. And, yet, our work exploring how we might unleash the potential of healthcare data whilst harnessing its value has long-since recognised the shifting sands that amount to ‘information governance’ in the UK health and care landscape; a situation rendered infinitely more complex by the known unknowns implied by Brexit. It has also, always, recommended transparency and recourse to the highest ethical standards to build and maintain public trust proactively in healthcare data usage.
Most recently, our collaboration with the National Consortium of Intelligent Medical Imaging (NCIMI) to support the development of a framework for fair value distribution amongst healthcare data subjects, controllers and processors has involved our working with Anthony Collins Solicitors LLP to undertake an analysis of the legal provisions and issues impacting research and commercial usage of healthcare data. That the resultant Review constitutes a detailed and lengthy exposition is, in and of itself, indicative of attendant complexities. Establishing solid foundations for data-driven research and innovation in healthcare is, then, a highly unusual business – even when we concern ourselves with conducting business as usual.
Research and Commercial Use of Medical Images – for today and tomorrow
We need an understanding of the operating context to help us develop strategies to achieve our goals. In the case of NCIMI, this goal is to support the NHS, academic and commercial parties to collaborate effectively and ensure healthcare data (specifically, medical imaging data) can be harnessed to deliver solutions which will improve care for patients in the UK and beyond. This was a ‘peacetime’ goal for NCIMI such that a range of projects were underway across cancer, cardiovascular disease, metabolic and women’s health before the public health emergency was declared. The time-critical nature of the pandemic has, however, required the Consortium to pivot and respond to urgent needs against a backdrop which is complex, even to those with expertise and experience in navigating the nuances.
Our legal Review with Anthony Collins Solicitors has provided a basis for discussion across different stakeholders both at a national level and within NCIMI, mapping a route and prompting helpful questions to ensure a balance can be struck between the frequently opposing needs for innovation, pragmatism, safety and caution. This is a requirement amongst all those working across sectors with healthcare data – to consider the different value propositions of those working toward a common goal but with different individual roles to play. Rarely has this common goal seemed clearer than in the context of the pandemic, with commercial entities offering free solutions and collaborating with direct competitors, whilst the NHS is proving itself pragmatic and responsive to demand for broad-ranging healthcare data.
We hope that the benefits of these behaviours will be felt when we return to business as usual but, until then, we must ensure that we retain sight of the value of checks and balances in the context of our ‘new normal’. The Review raises questions that apply to both modus operandi and supports ongoing reflection and consideration of how research and the commercial exploitation of healthcare data can achieve the goal that sits at the heart of the activity – improving care for patients.